Teaching Clinical Empathy to Healthcare Professionals
Have you ever walked out of a doctor’s appointment feeling like your concerns weren’t heard or like you and the doctor were having two different conversations? Then you know just how much the doctor-patient relationship can have a huge impact on your experience in the healthcare system. The good news is that leaders in medical education are calling for more focus on empathy as a key component of a good patient experience. They agree with us that empathy can be taught, and are encouraging healthcare teams to cultivate it with their staff, and medical schools to include it in their curriculum.
Dr. Helen Riess of Harvard Medical School is one of these champions of empathy, telling UC Berkeley’s Greater Good Magazine that an integral part of healing is making the patient feel like their experience is human and relatable. This concept, called Self Psychology should be applied to all doctor-patient situations. “Although of course you need other techniques, if you don’t have that connection [with the patient], you don’t get anywhere” says Riess.
How is Empathy in Healthcare Defined?
Dr. Jodi Halpern points out that clinical empathy looks different than empathy in a broader context. In most cases, the doctor has not had a similar experience to the experience of their patient, so when thinking about empathy in healthcare, “empathy is an intellectual rather than emotional form of knowing.” Riess agrees that doctors should employ “cognitive empathy,” an understanding of what the patient is feeling and thinking, regardless of whether he or she has faced a similar situation.
Cognitive empathy helps doctors to maintain their clinical judgement, while still making patients feel that their feelings are recognized and addressed. Whether that means providing some tips and reassurance to someone who is afraid of needles, or showing with body language that this patient is a priority and that you are there to answer their questions, a little bit of clinical empathy can go a long way. Reiss also emphasizes that the cognitive empathy approach is preferable, to one where the physician “empathize[s] too much with that emotional fear”, both in the interest of the patient and the doctor.
The Benefits of Empathy in Healthcare
But besides the warm fuzzy feelings, does clinical empathy actually pay off? We’re not at all surprised that the answer is yes! Empathetic doctors are more attuned to patients’ emotions, and therefore tend to deliver not just more caring treatment, but more accurate diagnoses.
Empathy can also help to build trust between the doctor and patient, making the patient more likely to follow the doctor’s recommendations or instructions. For example, taking medication as prescribed makes them more effective, but only 50% of patients do so While trust and good communication are only one piece of improving adherence, we know that people put more stock in directions and advice from people that they trust. Research from the University of Glasgow shows that “empathetic therapeutic encounters are associated with better outcomes.”
Unlock innovation at your organization by developing empathy in your Healthcare team
Book an Empathy Toy workshop today
Learn MoreAnd empathy doesn’t just help patients; doctors benefit too! This study shows that when a patient feels their doctor is ignoring their emotional concerns in an appointment or interview, they’re likelier to raise the topic again, “sometimes repeatedly and with escalating intensity.” Not only is this a waste of time on both sides, but it’s also a lot less comfortable for the doctors, increasing stress in the workplace, which no one needs. When a physician invites a patient to talk about his or her emotional state and then validates those feelings, the patient-physician relationship is strengthened and both people are likely to walk away less stressed or upset.
Social-Emotional Skills: Their Stock is Rising
The good news is that more organizations are seeing the value of empathy in healthcare. Both the Liaison Committee on Medical Education (LCME) and the Accreditation Council for Graduate Medical Education (ACGME) say that interpersonal communication skills and leadership capabilities are essential requirements for becoming a doctor. Medical schools are also following suit, with Johns Hopkins Medical School implementing mandatory “courses and seminars that teach students to communicate with compassion and empathy” and the Medical College Admission Test (MCAT) has included “questions involving human behaviour and psychology” since 2015, to determine whether you get into med school at all.
The Challenges of Empathy in Healthcare
Just because empathy is recognized as being important, People have also pointed out that it can be hard to develop and prioritize.
Health policy expert Thomas H. Lee writes about the challenge that doctors face in the face of increased specialization. As they focus more on narrow fields of expertise, they can often overlook that their patients are suffering, and not just physically. Complex medical issues can lead to fear, uncertainty, and confusion for patients. Lee stresses that combining advanced science with empathic care can help build health systems that are efficient and have positive outcomes for the physical and emotional health of the patient.
Using the Empathy Toy to help Healthcare Teams Cultivate Empathy
Twenty One Toys believes in seeing the whole person, not just a problem. We’ve been fortunate to work with healthcare teams a across North America (including the Valley Health Team in California, St. Joseph’s Hospital in Toronto, and Toronto’s Sheridan College School of Applied Health), as well as with individual practitioners in occupational therapy and community health. These partners share our vision that it takes practice for doctors to effectively integrate empathy, given that they are trained to be experts in the diagnosis of problems. The Empathy Toy acts as a tool to help healthcare providers explore how a focus on diagnosis and specialized areas of medicine influences their ability to empathetically connect with their patients.
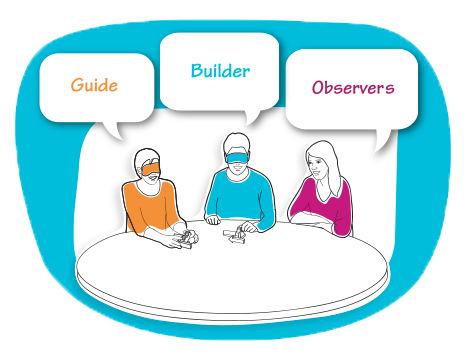
One of our favourite experiments to run during an Empathy Toy workshop involves comparing the outcomes of two games. In both, one player is designated as a ‘guide,’ the other as a ‘builder.’ The two must work together to complete a task, with the guide giving instructions to the builder.
Here’s the Difference:
-
In Game 1, both the guide and the builder are blindfolded. The guide still provides instructions to the builder.
-
In Game 2, the guide removes their blindfold, while the builder remains blindfolded.
In Game 1, both guide and builder experience similar feelings of uncertainty, so we often see that:
The guide acknowledges the challenges and frustrations of the game.
The guide actively seeks to collaborate with the builder by asking questions and soliciting feedback – especially when things aren’t going well.
The builder asks the guide a number of questions, unprompted.
The guide and builder use humour to defuse their shared sense of frustration.
Even if their results are imperfect, both players express satisfaction with the game.
By contrast, in Game 2, the guide, who can see the problem this time takes on the role of ‘expert.’ The instructions might be more accurate and specific, but we often see that the disparity between their experiences often drives a wedge between them. This happens for several reasons:
The guide is only focused on the problem, and not on emotionally supporting the builder.
The guide uses more complex language and is less likely to acknowledge how difficult the task is for the builder.
The builder asks fewer questions or seek clarification because they assume that the guide has better information, even if they don’t have related experience.
The guide rarely asks the builder for help.
Humour is used less frequently by both players.
Both players report feeling anxious about their roles and isolated in their frustration.
By playing, healthcare providers get to see some of the habit and assumptions that they have, and can practice them in a low risk task. It can also remind them of the “valuable time spent talking with patients” and the pitfalls of the “more-work-no-play mentality” that Riess says can be detrimental to the well-being doctors.

“[Using] the Empathy Toy was a great way for our team to deepen our understanding of how we communicate, and how our communication styles change depending on the different roles we play,”
– Irving Hernandez, Patient Experience coordinator at Valley Health Team
We know that healthcare needs to be more empathetic. The good news is that empathy is a highly teachable skill. As word about the benefits of empathy to both doctors and patients spreads, we’re excited to see a healthcare system that’s more compassionate, holistic and human.
Share your thoughts with us on twitter or send us a message!

